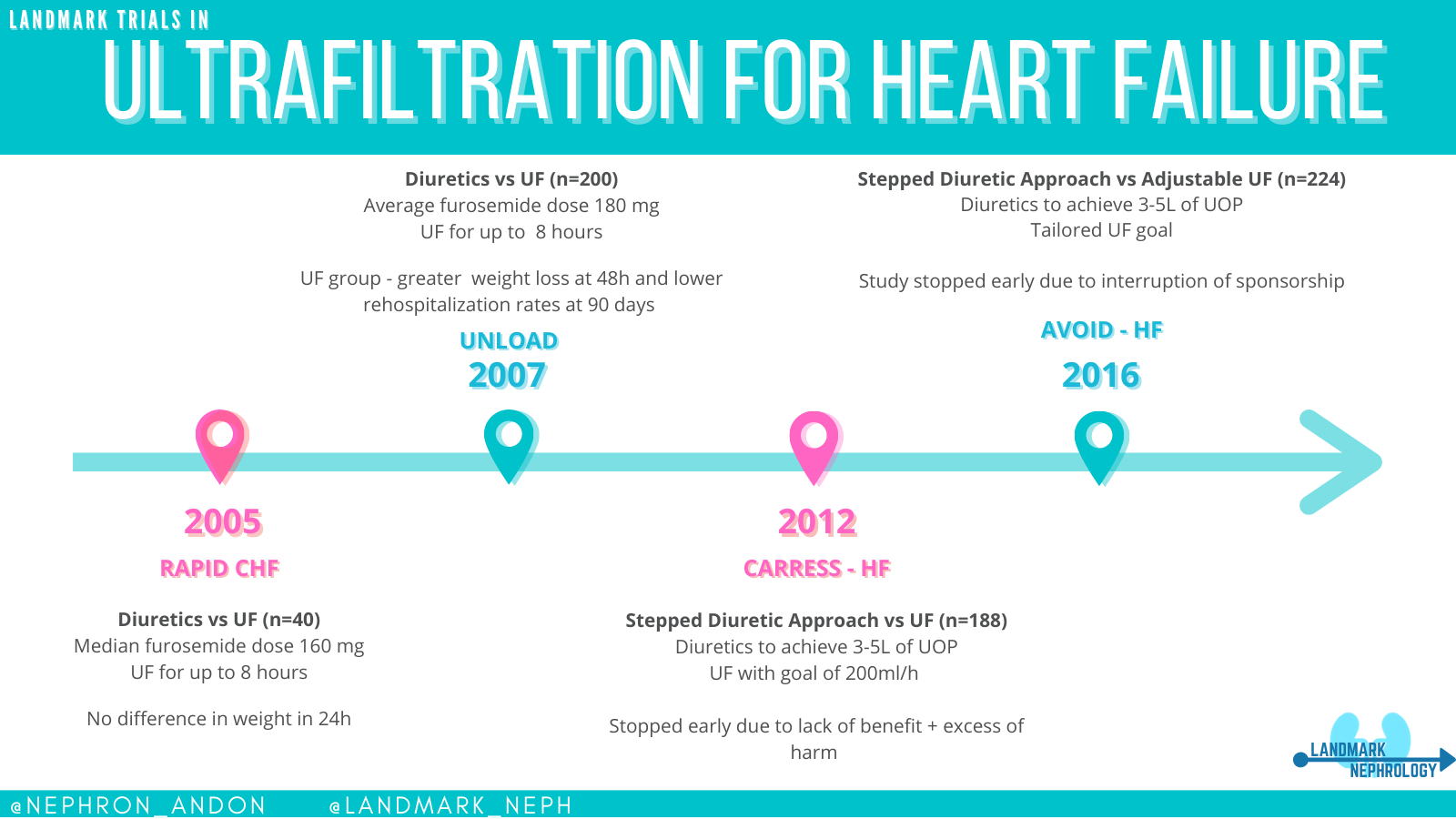
LANDMARK TRIALS IN
Ultrafiltration in HF
Diuretics
vs
UF
Diuretics
vs
UF
Stepped Diuretic Approach
vs
UF
Stepped Diuretic Approach
vs
UF
Hemofiltration in Heart Failure Patients
Posted on RFN : January 9th 2020
Updated: January 2020
The idea of removing fluid via ultrafiltration (UF) is not a new one. The first described use of UF dates back to 1974. Back then, drip clamps were used to calibrate the amount of UF. For this experiment, 5 patients underwent UF while also undergoing iHD, but the authors suggested that UF could be used in patients that did not require hemodialysis as well.
The role of UF in patients with volume overload has been largely studied since, especially in the heart failure (HF) population. Initially, the thought was that UF could remove volume more quickly then IV diuretics, impacting the patient possibly in a positive manner.
RAPID-CHF tried to establish the safety for UF in CHF patients and if it could lead to quicker fluid loss than diuretic use alone. 40 patients were divided in 2 groups of either diuretics only vs UF +diuretics and the primary end point was weight loss at 24h. The UF group received a single 8 hour session of UF. The average Cr in the UF group was 1.6 and 1.8mg/dL in the diuretic only group. At 24h, the UF group was 2.5 kg and 1.8 kg in the diuretic group but this difference was not statistically significant. The median diuretic dose for the diuretic only group was 160 mg, which is somewhat standard in cases with significant volume overload. One patient developed a catheter associated infection in the UF cohort. At the time, the group stipulated that the results for weight loss were likely not significant given the small sample utilized in the case.
Next, came UNLOAD. With a larger study group (now 200 patients enrolled), this trial compared UF vs diuretics, but now the primary endpoint were weight loss and dyspnea after 48h. They did follow kidney function as a safety outcome. Mean Cr was 1.5mg/dL at enrollment in both groups. UF treatments were conducted up to 8h at a time. After the first 48h, weight loss was greater in the UF group – with 5.0 vs 3.1kg loss (p0.001. The 90-day rehospitalization rate was also lower in the UF group. As far as adverse events, one case of catheter related infection was reported along with one patient developing renal failure in the UF group. In the diuretic only group, the average furosemide-equivalent daily dose was 180mg – which again, can be arguable seen as conservative.
CARRESS-HF then showed a different picture. They randomized patients to either UF only or what they called a “stepped pharmacology therapy”. UF rate goals were 200 ml/h of fluid removal. The goal of the pharmacological therapy arm was to achieve 3-5L of diuresis with loop and thiazide diuretics. The plan was to randomize 200 patients, however, after the enrollment of 188 the study was stopped given no signs of benefit and excess of adverse events with UF(72% vs 57% in diuretic group). The primary endpoints were change in weight and serum Cr at 96h from enrollment. The UF group had a statistically significant worsening in Cr when compared to the pharmacology group and the change in weight was similar in between the two groups. The rate of death or rehospitalization was also not statistically significant.
Critics of CARRESS-HF mention the fact of a predetermined rate of filtration during UF and a perceived delayed enrollment of some patients (average time from admission to enrollment was 34h) might have skewed the results. It is also important to mention that in this trial patients had a higher Cr (2.0mg/dL) than previous studies.
To try to overcome these critiques, the AVOID-HF trial was designed to compare adjustable UF rates versus diuretic treatment. This was one of the larger randomized trials in this subject – involving up to 810 patients which were randomized within the first 24 hours of admission. The primary outcome here was time to HF event within 90 days of discharge. The study ended up enrolling only 224 patients and was stopped by the sponsor due to slower than expected enrollment. The results from the study showed a trend towards longer time free from HF event on the UF group, but this was not significant. It is important to mention that serious adverse events deemed to be related to study therapy occurred in a higher number of patients in the UF group rather than in the diuretic group.
In summary, the data at this moment seems to point that there is more risk than benefit when using UF as a strategy for volume management in patients which do not have refractory volume overload, advanced renal failure or another indication for dialysis. For these lower risk patients, diuretics will always be safer. The remaining issue at hand is how to manage higher risk patients and whether early dialysis initiation versus aggressive cardiology care (e/g/ ionotropes) has better outcomes as both therapies have a high mortality rate at 1 year. Currently, the American College of Cardiology does not recommend UF as a first line treatment for HF.
Post By: Larissa Kruger, MD
Reviewed by: John Danziger, MD
ARTICLES
- Treatment of severe fluid overload by ultrafiltration.
- Ultrafiltration is associated with fewer rehospitalizations than continuous diuretic infusion in patients with decompensated heart failure: results from UNLOAD.
- Continuous Ultrafiltration for Congestive Heart Failure: The CUORE Trial
- Ultrafiltration in decompensated heart failure with cardiorenal syndrome.
- Aquapheresis Versus Intravenous Diuretics and Hospitalizations for Heart Failure.